Career resources content posted on NEJM CareerCenter is produced by freelance health care writers as an advertising service of NEJM Group, a division of the Massachusetts Medical Society and should not be construed as coming from, or representing the views of, the New England Journal of Medicine, NEJM Group, or the Massachusetts Medical Society
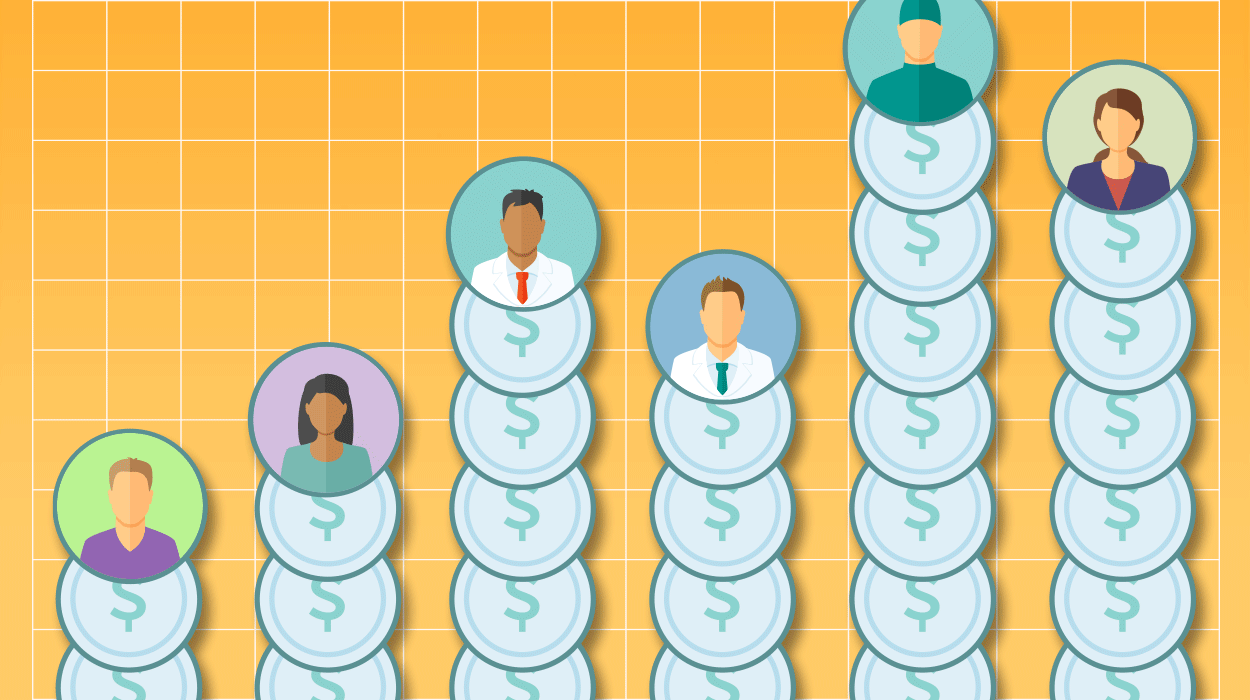
Earnings are increasing modestly, but a few specialties are seeing big hikes and others, flattening incomes
By Bonnie Darves, a Seattle-based freelance health care writer
Although the last two years have brought dramatic shifts in the health care delivery landscape — with the implementation of health-reform provisions and vigorous, often contentious debate on Capitol Hill about how to address the system’s intrinsic ills and contain costs — things have been relatively quiet on the physician-compensation front. Compensation continues to edge upward, generally, for most physician specialties, even if it’s leveling off in a few. In addition, there are no signs that an unbalanced supply-and-demand picture is producing unsustainable compensation increases in certain specialties, a pattern that occurred with relative frequency until a few years ago.
That doesn’t mean that there’s not much going on in physician compensation. There is a good deal of activity afoot that is starting to affect both physician compensation levels and structures, and will continue to do so in the years ahead. The trend toward hospital employment, which has taken off in the last two years, for example, is both a key factor and a challenge in compensation design now. This development is affecting income spreads on the spectrum, as hiring organizations discover that they must pay highly competitive rates to attract the physicians they need to ensure sufficient representation in all specialties.
“There’s a sense that some organizations are actually overpaying right now, for the market, as they try to catch up with hiring and build their physician networks,” said Travis Singleton, senior vice president at the national recruiting firm Merritt Hawkins. That means that some physicians just out of training are being paid nearly as much as their more experienced counterparts in some specialties, a trend Mr. Singleton and others in the industry expect will lessen as the hiring boom subsides.
On the national level, movement toward new payment methodologies for health services, such as the emergence of accountable care organizations (ACOs) and bundled payments for certain costly diagnoses and procedures, will soon affect compensation. “We’re seeing more factors such as cost of care, and quality metrics such as patient outcomes creeping into compensation design now — even in specialties where that hasn’t been as common, as in primary care,” said Brad Vaudrey, a principal with the independent consulting firm Sullivan, Cotter, and Associates, which produces the annual compensation survey for the American Medical Group Association (AMGA) and develops physician compensation programs.
1. This trend — particularly individual-physician performance metrics — hasn’t amounted to a substantial shift in physician compensation yet, Mr. Vaudrey observes, but he expects it soon will. “We will see more of this movement toward value- and outcomes-based physician compensation in the next few years,” he said. The cumulative effects of changing compensation components likely will become more pronounced, he added, as hospitals and large groups acquire practices or directly employ more physicians.
2. Even large physician organizations whose economic underpinnings are stable are anticipating these changes and are adjusting their compensation structures to respond to the changes ahead. “All of these developments — ACOs and bundled payments, and line-of-treatment plans — are designed to limit expense and improve care quality, but they also will affect physician compensation in the future,” said Richard Nesto, MD, executive vice president and chief medical officer for the Lahey Clinic in Burlington, Massachusetts.
The 520-physician clinic, one of the country’s largest practices, is revising its compensation structure to move toward leaner staffing and higher productivity, and to incentivize improved outcomes. “The base for what we get paid [as an organization] is shrinking, so we are preparing ourselves for the uncertainty out there,” Dr. Nesto said. “We are working to make our physicians more aware of the finances of the organization because some specialists, I think, have unrealistic expectations regarding earnings,” he said.
Big Compensation Swings Less Common
In the interim, there are several notable trends in physician compensation. The most pronounced one is that compensation in the primary care specialties is catching up in a big way. Two of the leading physician compensation surveys, those produced annually by the Medical Group Management Association (MGMA) and the AMGA, reported significant jumps in those earnings last year, following a few years of more modest increases. The MGMA’s 2012 Physician Compensation and Production Survey reported a 5.16% median increase in annual primary care compensation, and AMGA’s 2012 Medical Group Compensation and Financial Survey reported an average 4% increase. In both surveys, family medicine saw the biggest gains: MGMA reported median compensation of $212,840, and AMGA a median of $219,362.
Pediatrics experienced a similar increase. AMGA reported a 6.14% jump in median compensation, to $203,948; the MGMA survey found median compensation of $220,644, a total increase of $17,812 since 2009. Internal medicine median compensation, $224,417, saw a more modest increase (2.24%) in the MGMA survey. The AGMA reported median compensation of $215,689, up 5.02% over the previous year.
“We are finally beginning to see primary care become more attractive from the compensation standpoint,” said Todd Evenson, director of data solutions for the MGMA, in Englewood, Colorado. “The acquisition of physician practices is driving some of this, but it’s also the regulatory environment, particularly the recognition of the larger role primary care will play in the post-reform environment.”
The picture was more mixed in the specialties. Both the medical specialties and surgical specialties experienced compensation increases, ranging from approximately 2% to just over 10% across all specialties. The most dramatic year-over-year increases in the MGMA survey were in emergency medicine, at 8.43%; a 7.37% increase in hematology/oncology; and an 11.99% jump in urology.
In the AMGA survey, dermatology median compensation increased 13.33% and hospitalist compensation 11.64%, to $236,500. Urgent care physicians saw their compensation increase 5.17%, to a median of $242,145 in that survey’s findings. Following are other trends the surveys identified:
- Flattening compensation for invasive cardiology, endocrinology, infectious disease, neurology, radiology, and psychiatry — all of which saw increases of 2% or less.
- In the surgical specialties, orthopedics saw a large increase: 5.25% in MGMA data, to a $541,684 median compensation; and 2.78% for AMGA, with the median at $515,759. Ophthalmology posted a 7.04% increase in the MGMA survey, to a median compensation of $354,063.
- General surgery compensation increased only 0.74% (AMGA) to $370,024. Neurosurgery was flat in MGMA’s findings — at $740,702 median overall and $468,188 in academic neurosurgery. The AGMA median in neurosurgery was $656,250.
- In discretionary compensation, patient satisfaction and clinical outcomes are the key contributing components practices are using now — at 46% and 28%, respectively, according to AMGA respondents. Interestingly, seniority has all but dropped off the map in that regard; only 3% of respondents used that as a compensation determinant.
Geographic variations in physician compensation continue to follow the pattern demonstrated over many years: Physicians who practice in the South have the highest median compensation, and those in the Eastern region the lowest. For example, the MGMA reported median compensation for primary care specialties of $223,456 in the South in 2011, versus $206,344 in the Eastern region; the regional compensation spread for the specialties in those two regions was $419,487 and $353,100, respectively.
Despite the major changes going on in health care, physicians coming out of training — both primary care physicians and specialists — will continue to see a vibrant market for their skills, and stable compensation, especially with the aging population, according to Mr. Vaudrey. “Even though we are starting to see net decreases in revenues for groups, there has been an increase in demand for physician services, especially in the surgical specialties,” he explained.